Non-small cell lung cancer (NSCLC), including adenocarcinoma and squamous cell carcinoma subtypes, is a leading cause of cancer deaths worldwide. Treatment of NSCLC has advanced from chemotherapy modalities to the use of immunotherapy, namely immune checkpoint inhibitors (ICIs) which enhance the adaptive immune response against tumour cells. Thus, while the immune cell composition of tumours and its influence on treatment outcomes is poorly understood, it likely holds the key to effective, personalized treatment regimens.
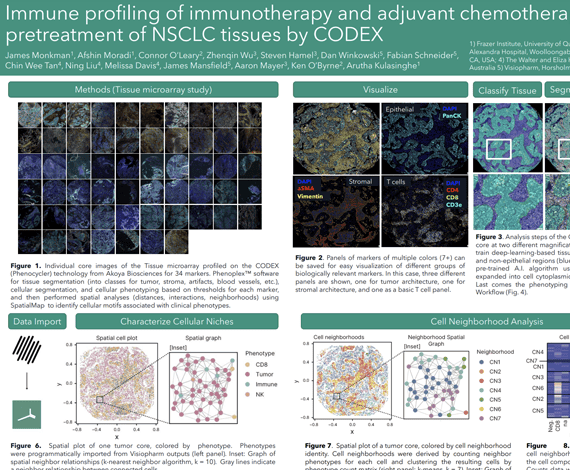
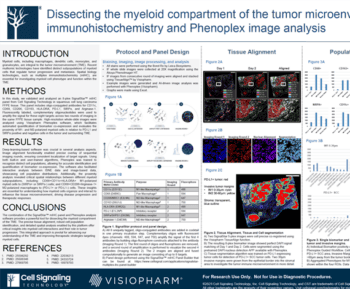
Here we profiled an adjuvant chemotherapy (n=61) as well as a second line immunotherapy (n=42) NSCLC cohort by the Phenocycler CODEX technology (highplex spatial proteomics) to investigate the association between immune composition and patient outcome. We applied a panel of 38 markers to delineate naïve, memory, cytotoxic and hyperactivated T cell states, as well as B cells, Tregs and myeloid lineage innate immune cell types. Our study sought to understand the heterogeneity of tumour-immune composition across patients and investigate the spatial neighbourhoods and clusters that these cells inhabit within TMA cores. We used Phenoplex™ software for tissue segmentation (into classes for tumor, stroma, artifacts, blood vessels, etc.), cellular segmentation, and cellular phenotyping based on thresholds for each marker, and then performed spatial analyses (distances, interactions, neighborhoods) using SpatialMap1 to identify cellular motifs associated with clinical phenotypes.
Our study has identified spatial features associated with immune contexture linked to therapy outcome in both chemotherapy and immunotherapy modalities. Taken together, our study demonstrates the utility of spatial proteomics to identify cellular features associated with outcome to therapy in lung cancer.
James Monkman1, Afshin Moradi1, Connor O’Leary1, Zhenqin Wu2, Steven Hamel2, David Mason3, Fabian Schneider3, James Robert Mansfield3, Aaron Meyer2, Ken O’Byrne4, Arutha Kulasinghe1
- The University of Queensland, Brisbane, Australia
- Enable Medicine, Menlo Park, CA
- Visiopharm, Horsholm, Denmark
- The Princess Alexandra Hospital, Woolloongabba, Australia