The importance of stain quality
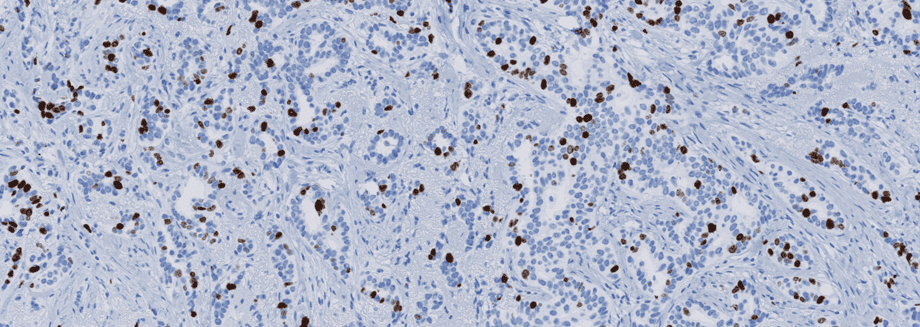
Immunohistochemical staining of tissue slides is a powerful tool that can provide pathologists and clinicians great insight for diagnosis, prognosis, and treatment of many disease states, particularly cancer.
However, like most tools that offer such significant benefits, it doesn’t come without challenges. The quality of staining in immunohistochemistry is an essential factor that may limit its effectiveness as a clinical tool. To correct the quality issues, it is vital to first understand how quality issues arise.
Stain quality can be described in terms of a signal-to-noise ratio (SNR), where signal refers to the level of expected epitope staining, and noise is the background component that results from cross-reactions with undesired epitopes. Insufficient SNRs are commonly the result of using poor or nonrobust antibodies and improper calibrations, the result of which mostly are false negative tests. Careful consideration for proper controls and adherence to quality control within the lab performing the staining protocol must be a priority to achieve optimal stain quality.1
An underlying reason for the variable quality being delivered by labs is the inherent complexity of an immunostaining protocol. Not only are protocols constantly being optimized, but with over 50 steps, each with multiple options, the staining protocol can have millions of variations. This has made standardization difficult.
One study conducted by the Nordic Immunohistochemical Quality Control (NordiQC) found an error rate in staining of almost 30% in labs participating in their study.
One study conducted by the Nordic Immunohistochemical Quality Control (NordiQC) found an error rate in staining of almost 30% in labs participating in their study.2 Dr. Vyberg, an expert in immunohistochemical quality control, noted that one reason for this high error rate is the use of in-house or “home-brew” kits rather than ready-to-use kits, which has direct consequences for treatments. Labs avoiding ready-to-use kits to save money on the front end could actually end up costing hospitals more in the long run.
An example is in the detection of the HER2 protein in breast cancer, one study calculated that every $1 labs saved by using in-house kits for HER2 rather than ready-to-use kits cost the hospital $6.3 However, quality assessment organizations have no authority to enforce underperforming labs to change their protocols.
This is not to suggest that all ready-to-use products are error-proof; internal standardization within each operating lab is critical with the use of any kit. Additionally, the field must be aware of the constantly evolving methods of staining in order to adopt the best possible protocols.
Early detection for some cancers is critical; delay in diagnosis and treatment increases the death rate considerably.4 Immunohistochemistry has the potential to help in early cancer detection, but first, the issue of stain quality must be addressed. One effort that is currently being made by NordiQC is the transparent sharing of optimal protocols for widespread use on their website. However, awareness and additional efforts are still needed, as solutions to this problem could directly impact cancer patients across the world.
1. Vyberg, M. & Nielsen, S. Proficiency testing in immunohistochemistry—experiences from Nordic Immunohistochemical Quality Control (NordiQC). Virchows Arch. 468, 19–29 (2016).
2. Nielsen, S. External quality assessment for immunohistochemistry: Experiences from NordiQC. Biotech. Histochem. 90, 331–340 (2015).
3. Vyberg M, Nielsen S, Røge R, Sheppard B, Ranger-Moore J, Walk E, Gartemann J, Rohr UP, Teichgräber V. Immunohistochemical expression of HER2 in breast cancer: socioeconomic impact of inaccurate tests. BMC Health Serv Res. 2015 Aug 29;15:352. doi: 10.1186/s12913-015-1018-6.
4. Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-JonescE, O’Sullivan DE, Booth CM, Sullivan R, Aggarwal A. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020 Nov 4;371:m4087. doi: 10.1136/bmj.m4087.



